Introduction
Human papillomavirus (HPV) infection is a common sexually transmitted disease caused by human papilloma virus. Almost 50% of sexually active adults have been infected genital HPV types and most infections have sub-clinical manifestations. As HPV and cervical cancer are found to be associated together, early prevention and treatment of human Papillomavirus infection should be done.
Human Papillomavirus (HPV)
- Human Papilloma Virus (HPV) was the first known human tumor virus.
- HPVs are non-enveloped, double-stranded DNA viruses and is resistant to ether inactivation, freezing, and desiccation.
- The double-stranded DNA genome consists of 3 main regions.
| Regions | Function |
| Early Region (E) | Encodes genes necessary for viral cycle and cell transformation |
| Late Region (L) | Encodes the L1 and L2 capsid proteins |
| Upstream Regulatory Protein | Regulates DNA replication by controlling viral gene transcription |
- The HPV genome encodes 6 early-open reading frames (E1, E2, E4, E5, E6, E7) and 2 late-opening reading frames (L1, L2).
- Among the identified more than 120 distinct HPV subtypes, 30 HPV types infect the genital epithelium.
- HPV infecting keratinocytes can have clinical manifestations of warts.
The risk associated with HPV genotypes:
Low-risk HPV
- It includes HPV types 6, 11, 42, 43, 44, 53, 57.
- Among these low-risk HPV types, HPV types 6 and 11 are the most common cause of genital warts.
- Low-risk HPV causes anogenital warts and low-grade cervical lesions.
Intermediate-risk HPV
- It includes HPV types 31, 33, 35, 39, 45, 51, 52, 55, 56, 58, 59, 68.
- They are the common cause of squamous intraepithelial neoplasia and less common causes of squamous cell carcinoma.
High-risk HPV
- It includes HPV types 16, 18
- They are strongly associated with cervical dysplasia and anogenital cancer.
- It is estimated that all cancers worldwide are attributable mainly to high-risk HPVs, including HPV types 16, 18, 31, 33, 35, 39, 45, 52, 52, 56, 58, and 59.
Incidence
- The lifetime risk of acquiring HPV infection is estimated to be at least 50%.
- It is estimated that about 2 million new cases of HR-HPV infection occur in the US each year.
- At any given time, around 20 million Americans have an HPV infection.
- The highest rates of genital HPV infection are found among adults of 18-28 years of age.
Factors Affecting HPV Infection
- Viral load (Number of viral lesions in the lesions contacted)
- Viral type
- Degree of exposure to the lesion
- Host’s defenses against HPV Infection
- Environmental factors
Diseases associated with HPV Infection
- Common wart
- Flat (plane) warts
- Plantar warts
- Epidermodysplasia verruciformis
- Anogenital warts
- Anogenital cancers and precancer
- Oral lesions
Warts
- Warts are non-cancerous (benign), rough, keratotic papules that may appear singly or grouped on any cutaneous surface caused by HPV.
- It is mostly located on dorsal aspects of hands and fingers.
- Histologically, warts are benign lesions with hypertrophy of all layers of dermis, resulting in acanthosis (thickening), papillomatosis (folding) and hyperkeratosis (increase in the horny layer) often with keratohyalin granules.
- Common warts are most commonly due to HPV 2, HPV 4
Sign and Symptoms
- Most people who acquire HPV infection are asymptomatic.
- Approximately, 90% infections of HPV are low-grade, non-oncogenic disease that resolves within 2 years and only 1% progresses into invasive cancer
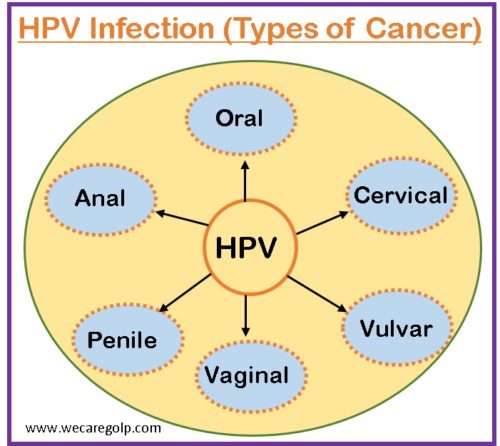
- HPV infection is associated with almost all cervical cancers and most of anogenital (vulvar, vagina, penile, and anal) and oropharyngeal cancers.
- It is also associates with other skin and mucosal lesions such as warts and benign papillomas.
The clinical lesions due to HPV infection can be divided into two broad categories.
Cutaneous manifestations
- Common warts (Verruca Vulgaris)
- Filiform warts (Verruca Filiformis)
- Flat warts (Verruca Plana)
- Plantar warts (Verruca Pedis)
- Anogenital warts
- Bowenoid papulosis
Extracutaneous manifestations
- Oral common warts
- Oral condylomata acuminata
- Focal epithelial hyperplasia
- Oral florid papillomatosis
- Nasal papillomas
- Conjunctival papilloma
- Laryngeal papillomatosis
- Cervical warts
Risk Factors
Behavioral risk factors
- Increased number of sexual partners
- Early age at first intercourse
- High frequencies of vaginal sex
- Smoking
- Oral contraceptive use
- Other STIs (chlamydia and herpes simplex virus)
- Chronic inflammation
- Immunosuppressive conditions
- Young age
- Hispanic ethnicity
- Black race
Socioeconomic risk factors
- Limited access to health care
- Low socio-economic health status
- Low educational status
- Poor reproductive health knowledge
- Low treatment coverage
- Low screening utilization
Mode of Transmission
Auto inoculation
- Immediate contact with hands through virus shedding in the anogenital regions (genital and oral sites)
Perinatal transmission
- Vertical transmission from mother to child in utero transmission
- Via placenta or umbilical cord
- During vaginal delivery
- At caesarean section
- Perinatally via breast milk
Inter site transmission between individuals
- Transmission during oral sex, anal sex, oral- oral contact (open-mouth kissing) or indirect transmission through contact with hands
- Vaginal-penile sex (most common route)
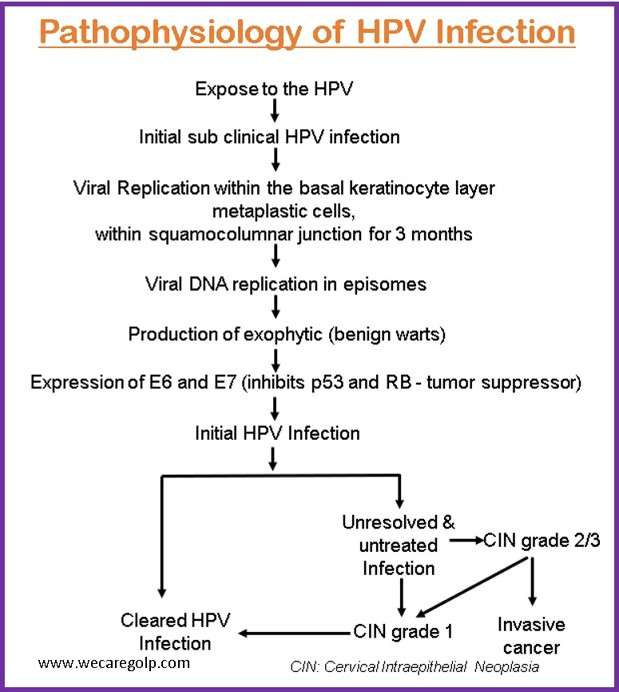
Pathophysiology
Diagnosis
HPVs cannot be cultured and HPV detection depends on the techniques used in immunology, serology, and molecular biology. However, techniques used for the diagnosis of HPV infection are;
HPV DNA testing
- Southern blots
- Dot blots
- In situ hybridization
- Polymerase chain reaction (PCR): most sensitive
- Solution hybridization (Hybrid capture assay)
Electron microscopy: for high resolution images of biological and non-biological specimens.
Serological assay (virus-like-particle-(VLP)-based enzyme immunoassays): not used clinically.
Screening test
- Pap smear: Precancerous cells and cervical cancer are detected during a Pap smear. High-risk HPV is almost always the cause of cervical cancer.
- HPV test: High-risk strains of the virus can be identified by HPV tests. Cervical cancer is detected using this method.
- Visual inspection with acetic acid (VIA): VIA is typically used when regular Pap smears and HPV tests are unavailable. A vinegar-based solution is applied to the cervix. The abnormal cells turn white.
- Colposcopy: If the Pap smear shows signs of abnormal cells or if the HPV test results positive, a colposcopy is performed. A colposcope, a light-emitting instrument, is used in this procedure to magnify your cervix and remove abnormal tissues. The removed tissues will be sent to a lab to detect the signs of cancer or precancer.
Treatment
The virus cannot be eradicated through treatment. However, any visible warts on your genitals and abnormal cervix cells can be treated. Treatment of HPV infection depends on the clinical manifestations and the potential for malignancy. Common treatment modalities used in the management of HPV infection are:
Pharmacological therapy
- Trichloroacetic acid: Chemical treatment that burns off warts
- Creams (Imiquimod, podofilox): For treatment of external genital warts
Physical Ablation
- Cryotherapy: Utilize liquid nitrogen to destroy abnormal cells or freeze warts.
- Laser therapy: Use a powerful light to kill warts and other abnormal cells.
- Conization (cold knife cone biopsy): Remove a piece of abnormal cervical tissue in the shape of a cone.
- Electrocautery: Remove warts by burning them with electricity.
- Loop electrosurgical excision procedure (LEEP): Remove cervix warts or abnormal cells with a special wire loop.
Complications
- Cutaneous wart
- Anogenital warts
- Oropharyngeal cancers
- Anogenital cancer (vulvar, vaginal, penile cancer)
- Cervical intraepithelial lesion (CIN)
- Cervical cancer
Prevention
Vaccination
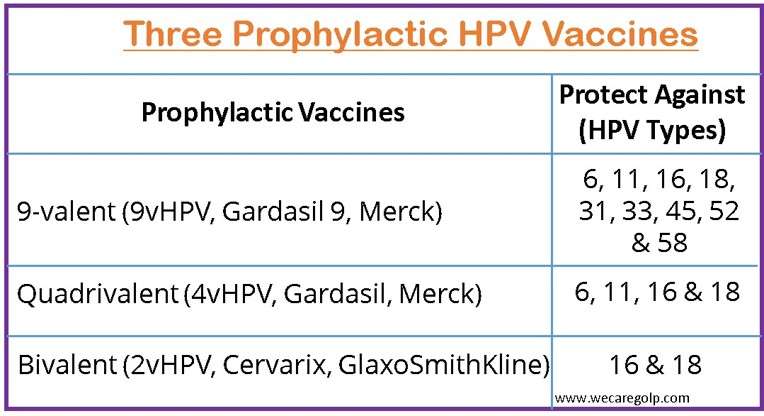
- The vaccine can protect HPV infections including cancers. People who experience high efficacy of the HPV vaccine are those who have not been exposed to vaccine-type HPV prior to vaccination.
- The vaccine is recommended by the CDC for:
- All preteens (both boys and girls) between the ages of 11 and 12 (or as early as age 9).
- Everyone over the age of 26, if they haven’t already been vaccinated. However, HPV vaccination has fewer benefits for this age group.
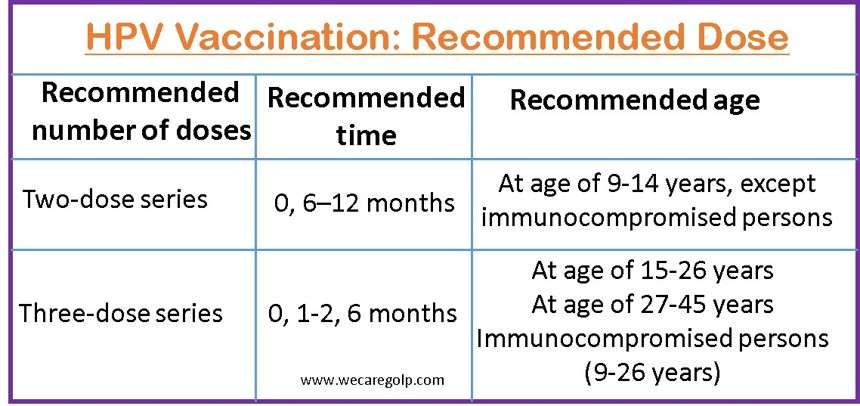
- Prophylactic HPV vaccinations prevent new HPV infections. The prophylactic vaccinations do not
- Prevent the progression of HPV infection to disease
- Shorten the time it takes to clear an HPV infection
- Treat HPV-related diseases.
Other Preventive Measures
- Use condom persistently during sex (vaginal-penile, or oral sex)
- Have only one sex partner
- Get screened for cervical cancer regularly (Cervical cancer can be avoided if women between the ages of 21 and 65 undergo regular screenings.)
- Wash hands thoroughly
- Educate people on prevention, risk factors and management of HPV Infection
Prognosis
- HPV infections resolve spontaneously in approximately 70% of cases within one year and in 90% of cases within two years. In other cases, HPV persistence can lead to various disease manifestations.
- It is estimated that HPV causes 85% of anal cancers, 50% of cancers of vulva, vagina, and penis; 20% of oropharyngeal cancers; and 10% of laryngeal and esophageal cancers.
Summary
- HPV infection is a common sexually transmitted infection caused by double-stranded, non-enveloped human papilloma virus.
- Among the identified more than 120 distinct HPV subtypes, HPV 16 and 18 are the high-risk HPV types.
- The clinical manifestations of HPV may be cutaneous or extra cutaneous lesions.
- HPV may be transmitted by auto inoculation, perinatal transmission and inter site transmission between individuals.
- HPV infections are highly related to the incidence of cervical cancer, cancers of the oropharynx, oral cavity, and the anogenital tract. So, prevention, early diagnosis and treatment of HPV infection should be highly emphasized.
References
- Cobb, M.W. (1990). Human papillomavirus infection. Journal of the American Academy of Dermatology, 22(4), 547-566. doi: 10.1016/0190-9622(90)70073-q
- Koutsky, L. (1997). Epidemiology of Genital Human Papillomavirus Infection. The American Journal of Medicine, 102(5A), 3-8. doi:10.1016/s0002-9343(97)00177-0.
- Forcier, M., & Musacchio, N. (2010). An overview of human papillomavirus infection for the dermatologist: disease, diagnosis, management and prevention. Dermatologic Therapy, 23(5), 458-476 doi: 10.1111/j.1529-8019.2010.01350.x
- Castellsagué, X. (2008). Natural history and epidemiology of HPV infection and cervical cancer. Gynecologic Oncology, 110(3), S4-S7. https://doi.org/10.1016/j.ygyno.2008.07.045
- Hathaway, J. K. (2012). HPV: Daignosis, Prevention, and Treatment. Clinical Obstetrics and Gynaecology 55(3); 671-680, DOI; 10.1097/GRF.0b013e31825caa36
- Kombe Kombe, A. J., Li, B., Zahid, A., Mengist, H. M., Bounda, G., Zhou, Y., & Jin, T. (2021). Epidemiology and Burden of Human Papillomavirus and Related Diseases, Molecular Pathogenesis, and Vaccine Evaluation. Frontiers in Public Health, 8. https://doi.org/10.3389/fpubh.2020.552028