What is gastroscopy or esophagogastroduodenoscopy or EGD?
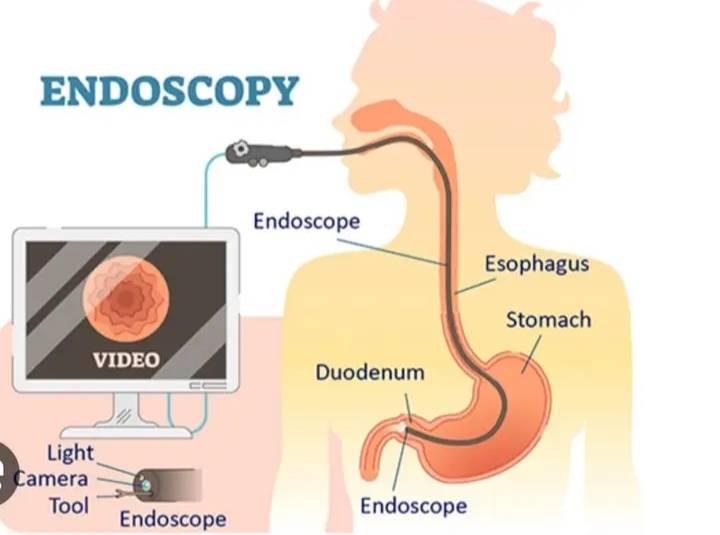
Gastroscopy or sophagogastroduodenoscopy (EGD) is an endoscopic procedure that allows gastroenterologists to examine the lining of the esophagus, stomach, and duodenum (i.e., the upper gastrointestinal or GI tract) using an endoscope. An endoscope is a flexible tube with a camera and a light at the end that is inserted through the mouth into the digestive tract. Gastroscopy or EGD can help diagnose various conditions affecting the upper gastrointestinal tract, including ulcers, gastritis, esophagitis, hiatal hernia, and Barrett’s esophagus.
What are the most frequent questions patients have about gastroscopy (EGD)?
One of the most frequent questions patients have about gastroscopy or esophagogastroduodenoscopy (EGD) is about the preparation for the procedure. Patients may be concerned about the dietary restrictions and bowel preparation needed before the procedure, as well as the discomfort associated with fasting and drinking the prep solution. Other common questions include what to expect during the procedure, how long it will take, and what the recovery period will be like. Patients may also have questions about the risks and potential complications of EGD, as well as how to prepare for sedation and what to expect after the procedure.
Discuss any questions or concerns you may have with your gastroenterologist prior to the procedure to ensure that you are fully informed and prepared.
Why is gastroscopy (EGD) performed?
Gastroscopy or esophagogastroduodenoscopy (EGD) is performed to diagnose and treat various conditions affecting the upper gastrointestinal tract, which includes the esophagus, stomach, and duodenum. Here are some of the most common reasons why EGD may be performed:
- Gastrointestinal Bleeding: EGD can help locate the source of gastrointestinal bleeding and sometimes even stop the bleeding by cauterizing the bleeding vessel or injecting medications.
- Ulcers: EGD can help diagnose peptic ulcers in the stomach or duodenum, and biopsies can be taken to determine if the ulcers are caused by H. pylori bacteria, which can be treated with antibiotics.
- Stomach Pain: EGD may be performed to diagnose the cause of abdominal pain, including inflammation of the stomach or esophagus, or the presence of a hiatal hernia.
- Difficulty Swallowing: EGD can help diagnose the cause of difficulty swallowing, which may be due to narrowing of the esophagus or the presence of a tumor.
- Gastroesophageal reflux: EGD can help diagnose gastroesophageal reflux disease (GERD) and other conditions that can cause acid reflux symptoms such as heartburn and regurgitation.
- Cancer: EGD may be performed to diagnose the presence of tumors in the esophagus, stomach, or duodenum, and biopsies can be taken to determine if they are cancerous.
- Unintended Weight Loss: EGD can help diagnose the cause of unintended weight loss by evaluating the upper gastrointestinal tract for conditions such as ulcers, tumors, or inflammation.
In summary, EGD is performed to diagnose various upper gastrointestinal conditions that can cause symptoms such as bleeding, ulcers, abdominal pain, difficulty swallowing, reflux symptoms, cancer, and unintended weight loss. The procedure is safe and generally well-tolerated, and patients should discuss any concerns or questions they have with their gastroenterologist.
Before the Procedure
Before the EGD, the patient is usually given sedatives to help them relax and avoid discomfort during the procedure. Follow your gastroenterologist’s instructions about fasting before the procedure to prevent complications during the procedure.
Avoid: eating for at least 8 hours, and drinking for at least 4 hours before the EGD.
During the Procedure
During the EGD, the patient is asked to lie down on their left side, and a mouthguard is placed in their mouth to protect their teeth and keep their mouth open. The endoscope is then passed through the mouth and into the esophagus, stomach, and duodenum. Air may be introduced into the stomach to improve visibility. The patient may experience some discomfort during the procedure, such as bloating, cramping, or nausea, but this is generally mild and short-lived.
The procedure usually takes between 15 and 30 minutes to complete. The doctor can take biopsies or remove polyps during the EGD, and these samples are sent to the lab for analysis.
After the Procedure
After the EGD, the patient is monitored for a short time to ensure there are no complications from the sedation. Patients may feel drowsy for a few hours after the procedure due to the sedatives. It is important to follow the doctor’s instructions about resuming normal activities, including eating and drinking.
Is gastroscopy or esophagogastroduodenoscopy safe?
Gastroscopy or sophagogastroduodenoscopy (EGD) is generally a safe procedure when performed by an experienced gastroenterologist or endoscopist. However, as with any medical procedure, there are risks and potential complications to consider. Here are some of the most common risks and complications associated with EGD:
- Bleeding: EGD can cause bleeding if the endoscope irritates or damages the lining of the digestive tract, or if a biopsy or therapeutic procedure is performed. Mild bleeding is common and typically stops on its own, but severe bleeding may require additional treatment.
- Perforation: EGD can cause a perforation (tear or hole) in the digestive tract, which can lead to infection, inflammation, and other serious complications. Perforation is rare, occurring in less than 1% of EGD procedures.
- Reaction to Sedation: EGD is typically performed under sedation, which can cause reactions in some patients. Common side effects of sedation include nausea, vomiting, dizziness, and headache.
- Infection: EGD can increase the risk of infection if the endoscope is not properly cleaned and sterilized between procedures. The risk of infection is low, but it can be serious in some cases.
- Aspiration: EGD involves the insertion of a tube into the mouth and throat, which can increase the risk of aspiration (inhaling food or liquid into the lungs). Aspiration is rare but can be life-threatening if it occurs. This is why EGD is never attempted when the patient has not fasted for several hours prior to the procedure.
These risks are rare and that most patients do not experience any complications from EGD. The benefits of EGD in diagnosing and treating conditions of the upper gastrointestinal tract generally outweigh the risks, and gastroenterologists take precautions to minimize the risk of complications.
Is gastroscopy (EGD) painful?
EGD is not painful, instead it is well-tolerated. Most patients undergo EGD without significant discomfort. Here are some factors that can influence the level of discomfort:
- Sedation: EGD is often performed with the patient under conscious sedation. This means you are given medications to make you relaxed and drowsy during the procedure. This can significantly reduce any potential pain or discomfort. Dr. Zavos performs endoscopies with the use of deep sedation and thus both gastroscopy and colonoscopy are completely pain-free.
- Local Anesthesia: Before the procedure, a local anesthetic may be sprayed or applied to the back of the throat to numb it, which can make it more comfortable. Dr. Zavos does not routinely use local anesthesia because deep sedation allows for the patient to sleep and not feel the insertion of the instrument.
- Patient Sensitivity: Some individuals may be more sensitive to the procedure than others. Factors such as anxiety or a heightened gag reflex can affect the perceived level of pain or discomfort. Deep sedation used by Dr. Zavos eliminates this factor.
- Condition Being Investigated: In some cases, the reason for undergoing an EGD may involve conditions that cause pain or discomfort, and the procedure itself might not be the primary source of pain. Again, deep sedation used by Dr. Zavos guarantees that the endoscopy is completely painless.
What are the advantages of gastroscopy compared to alternative diagnostic tests?
Gastroscopy or esophagogastroduodenoscopy (EGD) has several advantages over alternative diagnostic tests for evaluating the upper gastrointestinal tract. Here are some of the main advantages:
- Direct Visualization: EGD allows for direct visualization of the esophagus, stomach, and duodenum using an endoscope, which is a flexible tube with a camera on the end. This allows the gastroenterologist to see the tissues and structures in real-time and obtain biopsies or perform therapeutic procedures if necessary.
- Biopsy Capability: EGD allows the gastroenterologist to obtain biopsies of suspicious tissues or lesions in the upper gastrointestinal tract. These biopsies can be examined under a microscope to determine if they are cancerous or benign.
- Therapeutic Procedures: EGD allows for therapeutic procedures to be performed, such as the removal of polyps or the dilation of strictures (narrowed areas) in the esophagus, stomach, or duodenum.
- Accurate Diagnosis: EGD has a high accuracy rate for diagnosing conditions affecting the upper gastrointestinal tract, such as ulcers, tumors, inflammation, and Barrett’s esophagus.
- Lower Radiation Exposure: EGD does not involve the use of radiation, which is a benefit for patients who may be sensitive to radiation or who have already received high doses of radiation from other diagnostic tests.
While alternative diagnostic tests such as upper GI series, CT scan, and MRI may be useful in certain situations, EGD remains the gold standard for evaluating the upper gastrointestinal tract. The direct visualization, biopsy capability, therapeutic procedures, accuracy, and lack of radiation exposure make EGD a valuable diagnostic tool for gastroenterologists and their patients.
Is it possible to have a gastroscopy and a colonoscopy performed during the same session?
It is possible to have an esophagogastroduodenoscopy (EGD) and a colonoscopy performed during the same session, which is commonly referred to as an “upper and lower endoscopy.” This approach can be convenient for patients as it minimizes the need for multiple procedures and sedations.
However, whether or not both procedures can be performed during the same session will depend on several factors, including the patient’s medical history and current health status, the indication for the procedures, and the preferences and expertise of the gastroenterologist performing the procedure.
For example, if a patient has a history of bleeding disorders, it may be more appropriate to perform the procedures separately to reduce the risk of bleeding. Similarly, if the patient has underlying health conditions such as lung disease or heart disease, the gastroenterologist may prefer to perform the procedures separately to reduce the strain on the patient’s body.
How often can I have a gastroscopy?
The frequency with which you can have an esophagogastroduodenoscopy (EGD) depends on the reason for the procedure and your individual health status. In general, EGD is a diagnostic tool used to evaluate and treat conditions affecting the upper gastrointestinal tract, such as ulcers, inflammation, tumors, and blockages. Here are some guidelines regarding the frequency of EGD:
- Diagnostic EGD: If you are having an EGD to diagnose a specific condition, such as an ulcer or tumor, the frequency of the procedure will depend on the nature and severity of the condition. Once the condition has been diagnosed and treated, your doctor will determine if you need additional EGDs to monitor your condition.
- Surveillance EGD: If you have a history of certain conditions, such as Barrett’s esophagus, you may need regular EGDs to monitor for changes in the lining of the esophagus. The frequency of these surveillance EGDs will depend on your individual risk factors and the recommendations of your doctor.
- Therapeutic EGD: If you are having an EGD to perform a therapeutic procedure, such as the removal of a polyp or dilation of a stricture, the frequency of the procedure will depend on the success of the procedure and the likelihood of recurrence.
In general, EGD is a safe procedure and can be performed as often as necessary to diagnose and treat conditions of the upper gastrointestinal tract. However, because EGD involves sedation and carries a small risk of complications, it is important to discuss the frequency of the procedure with your gastroenterologist and ensure that the benefits outweigh the risks.
How can I contact gastroenterologist Dr. Zavos to arrange for me an appointment for an esophagogastroduodenoscopy or EGD?
Dr. Chris Zavos is a board-certified gastroenterologist and hepatologist, located in Thessaloniki Greece, and specifically in Kalamaria suburb, about 7 kilometres (4 miles) southeast of downtown Thessaloniki. His private office is at: Fanariou 8 street (near Aigaiou and Adrianoupoleos avenues), Kalamaria (Thessaloniki), Greece.
Thessaloniki International Airport is only 10 km away from his private office in Kalamaria and can be reached by taxi within 13 minutes from the airport.
Dr. Chris Zavos performs endoscopies at Bioclinic private hospital in downtown Thessaloniki (Mitropoleos 86 street).
You can contact Dr. Zavos at phone numbers: (+30)-6976596988 and (+30)-2311283833, or you can email him at czavos@ymail.com. Dr. Zavos responds to Greek and English languages.
